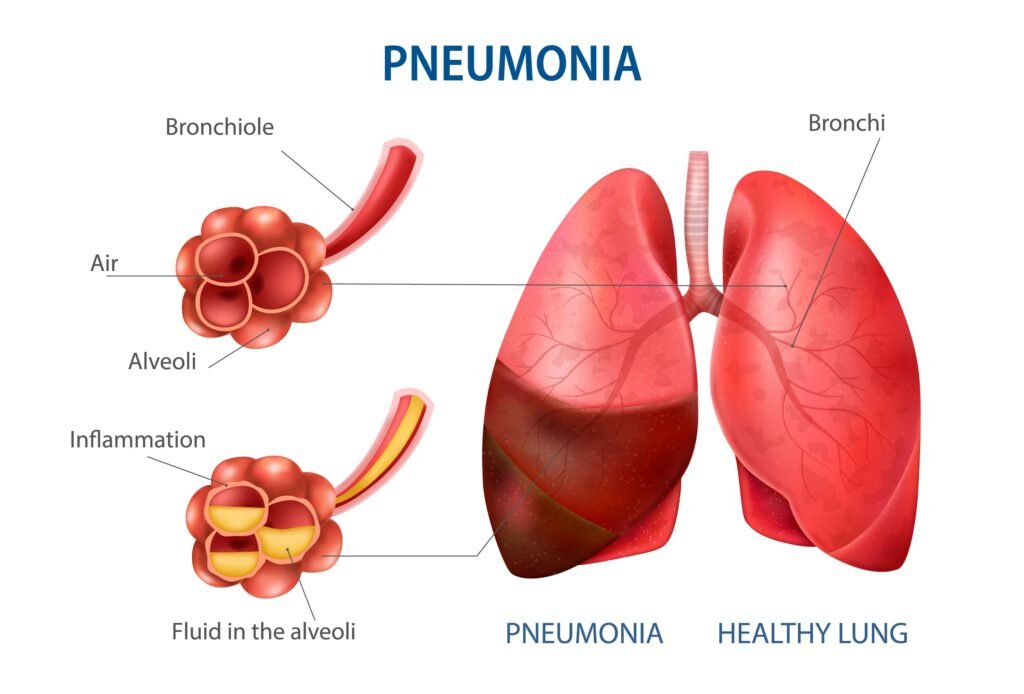
Pneumonia or lung inflammation is a condition that can occur not only in children but also in adults, although it is more common in infants and early childhood. Clinically, pneumonia can occur as a primary illness or as a complication of other conditions.
Learn more about pneumonia (lung inflammation) through the following discussion!
What Is Pneumonia?
Pneumonia is an inflammatory condition that occurs when someone has an infection in the air sacs of the lungs, a part of the human respiratory organs system. These infected air sacs fill with fluid or pus (purulent sputum). This disorder, one of the many diseases that attack the human respiratory organs system, can cause a productive or purulent cough, fever, chills, and difficulty breathing.
The infection caused by pneumonia can occur in one side of the lung or both. The main causes of this inflammatory disorder are infections from viruses, bacteria, or fungi. Pneumonia is commonly known as “wet lungs” in many countries. This disease can affect adults as well as children, even newborns.
Both viral and bacterial pneumonia are contagious diseases, meaning a person with pneumonia can spread it to others through inhaling airborne droplets from sneezes or coughs. Therefore, individuals with this condition should avoid spreading their oral fluids by wearing a mask.
Classification of Pneumonia
Here are the types of pneumonia based on the microorganisms causing the infection:
1. Bacterial Pneumonia
Bacterial pneumonia is pneumonia caused by a bacterial infection. This is the most common type of pneumonia, with the most frequent causative bacteria being Streptococcus pneumoniae.
A person can contract the bacteria causing pneumonia by inhaling droplets (small saliva particles) released by someone with pneumonia when they cough or sneeze. Infection is more likely if the person has a weak immune system, a history of lung disease, is a frequent smoker, or is recovering from surgery in the hospital.
2. Atypical Pneumonia
This type of pneumonia is also caused by bacteria, but its symptoms are milder than those of bacterial pneumonia. Because of its mild symptoms, people with pneumonia usually do not realize they are sick. This condition is referred to as walking pneumonia.
Atypical pneumonia is typically caused by Mycoplasma pneumoniae or Chlamydophila pneumoniae.
3. Viral Pneumonia
Various viruses can infect the lungs and cause this type of pneumonia. Viral pneumonia usually has a shorter duration than bacterial pneumonia and its symptoms are generally milder. However, viral pneumonia can sometimes be fatal, especially if caused by influenza virus, SARS-CoV-2 (COVID-19), or MERS. Children, the elderly, and those with weakened immune systems are at higher risk for fatal viral pneumonia.
4. Fungal Pneumonia
This type of pneumonia is caused by a fungal infection. Fungal pneumonia is rare and usually occurs in individuals with chronic diseases or weakened immune systems.
Examples of people susceptible to fungal pneumonia include those with AIDS, cancer patients undergoing chemotherapy, individuals with autoimmune diseases, or organ transplant recipients who must take immunosuppressive medications.
Causes of Pneumonia
The causes of pneumonia are varied, but based on the organism and the place of transmission, pneumonia is categorized into two types: community-acquired pneumonia, which spreads in the general environment, and hospital-acquired pneumonia.
Here are some categories of pneumonia causes:
- Community-Acquired Pneumonia
Organisms that cause community-acquired pneumonia differ from those in hospitals, with hospital-acquired organisms often being harder to treat.
Examples of organisms causing community-acquired pneumonia include:
- Bacteria, most commonly Streptococcus pneumoniae.
- Bacteria-like organisms, Mycoplasma pneumonia.
- Fungi, which typically affect individuals with weakened immune systems.
- Viruses.
- Hospital-Acquired Pneumonia
Some individuals can develop pneumonia while hospitalized for other conditions. This can be serious because the bacteria causing it may be more resistant to antibiotics and because the person is already ill. Those using ventilators, often in intensive care units, are at higher risk for this type of pneumonia. - Health Care-Acquired Pneumonia
This type of pneumonia occurs in people who have been in long-term care facilities or regularly receive care in outpatient clinics, such as kidney dialysis centers. Like hospital-acquired infections, this type is often caused by antibiotic-resistant bacteria.
Risk Factors for Pneumonia
Although it can affect anyone, some people are more vulnerable to pneumonia, such as:
- Children aged 2 years and under.
- Adults over the age of 65.
- Long-term hospitalized patients.
- Those in ICU and using ventilators.
- Individuals with chronic lung or heart disease.
- Smokers.
- People with weakened immune systems (e.g., HIV patients) or those on immunosuppressive medications, including chemotherapy.
Read More Ways to Keep Your Respiratory System Healthy
Symptoms of Pneumonia
The signs and mild symptoms of pneumonia generally resemble flu symptoms, such as fever and cough. These symptoms last longer than a typical flu. If left untreated, severe symptoms may develop, including:
- Chest pain when breathing or coughing.
- Productive cough with phlegm.
- Fatigue.
- Fever and chills.
- Nausea and vomiting.
- Shortness of breath.
- Confusion or changes in mental awareness (especially in those over 65).
- Hypothermia in those over 65 or with immune system disorders.
In children and infants, symptoms often include high fever, persistent fatigue, refusal to eat, productive cough, and shortness of breath, leading to rapid breathing.
Pneumonia Diagnosis
First, the doctor will ask about symptoms and medical history, including any unhealthy habits. Then, the doctor will listen to the sounds from the lungs. People with pneumonia often have crackling, bubbling, or rumbling sounds when they breathe in.
Some common tests performed by doctors include:
- Blood tests
- Chest X-rays
- Pulse oximetry
- Sputum tests
Additionally, more in-depth examinations may be necessary if a person has other health issues or is suspected of contracting pneumonia in a hospital. These tests include:
- Arterial blood gas test
- Bronchoscopy
- CT Scan
- Pleural fluid culture
The most frequent supportive examination is imaging, specifically chest X-rays. From the results, the doctor can identify the location of the infection. Blood lab tests are also conducted to determine the organism causing the infection.
Pneumonia Treatment
Treatment and management of pneumonia involve addressing the infection and providing supportive therapy.
The doctor will prescribe antibiotics to be taken until completed if the infection is bacterial. Supportive therapies may include:
- Fever reducers for high fever that disrupts daily activities
- Cough medicine to reduce coughing frequency or thin mucus
Hospitalization may be recommended if the following conditions are met:
- Age >65 years
- Altered consciousness
- Poor kidney function
- Very low blood pressure (<90/<60 mmHg)
- Very rapid breathing (over 30 breaths per minute)
- Below normal body temperature
- Pulse rate <50 or >100 beats per minute
Pneumonia Complications
Complications from pneumonia are more common in young children, the elderly, and those with pre-existing health conditions such as diabetes. Potential complications include:
- Pleuritis: Inflammation of the thin lining between the lungs and ribs (pleura), which can lead to respiratory failure.
- Lung abscess: A rare complication usually found in people with severe pre-existing illnesses or a history of severe alcohol abuse.
- Sepsis: Blood poisoning, a rare but serious complication.
Pneumonia Prevention
There are several ways to prevent pneumonia:
- Get Vaccinated
Vaccination is the primary way to prevent pneumonia. Ensure you are vaccinated to reduce the risk of this illness. Vaccines should be given to children, especially those under 2 years and those aged 2-5 years with different types of vaccines. Flu shots are also recommended for children over 6 months. - Maintain Hygiene
Practice good hygiene by regularly washing hands or using hand sanitizer to protect yourself from infections. - Quit Smoking
Stop smoking to ensure the protective mechanisms of the lungs are not compromised and remain effective against respiratory infections. - Maintain Immunity
Keep your immune system strong by getting enough sleep, exercising regularly, and eating healthy foods.